Prostate Biopsy Standards
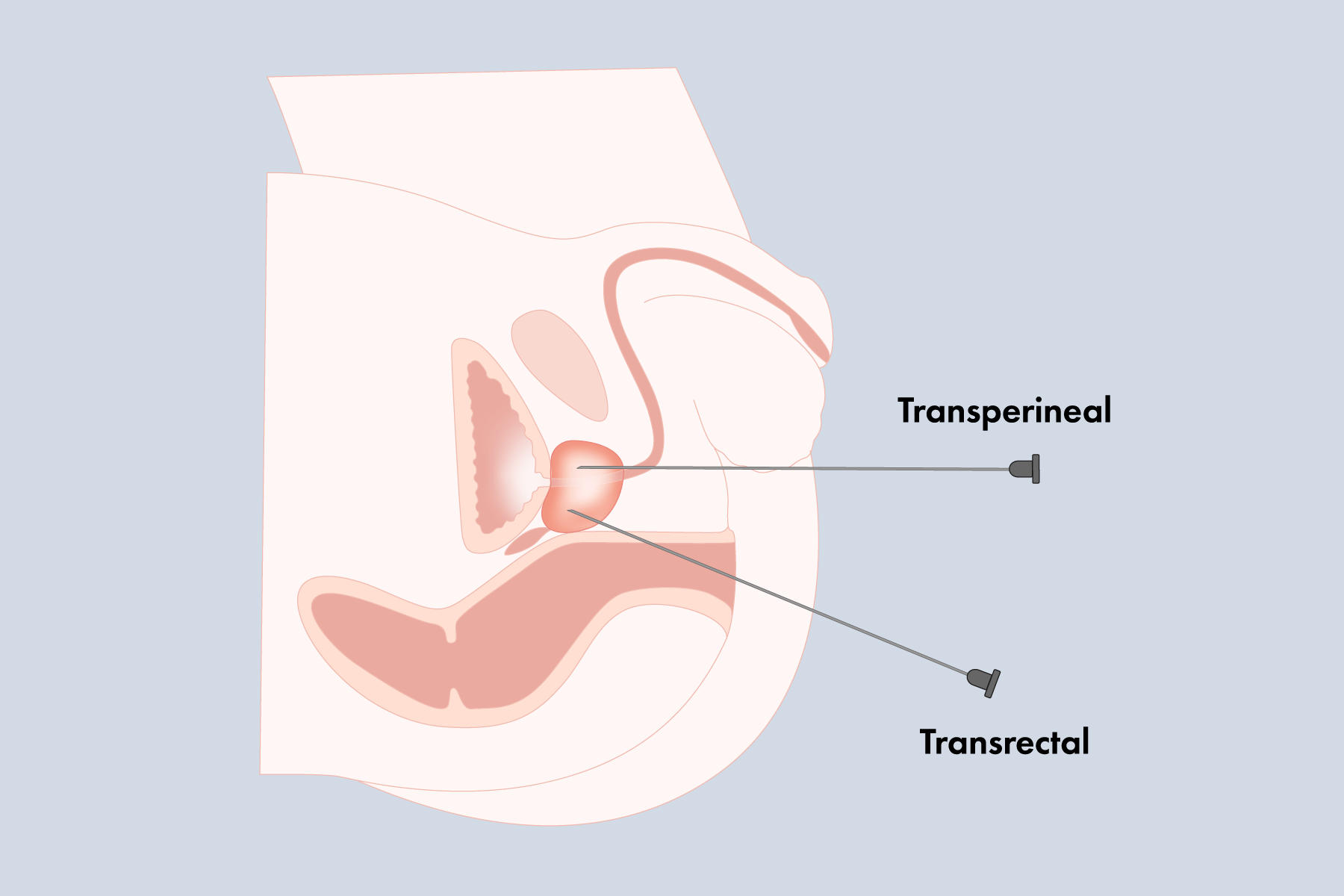
Although prostate cancer is the most commonly diagnosed cancer in men, the optimal method for diagnosis remains unclear. Favoured for its convenience and low cost, the systematic transrectal ultrasound guided biopsy is currently considered the gold standard for detecting prostate cancer, despite its high false negative rate and potential for infectious complications.1 The use of MRI improves the accuracy of detecting clinically significant cancer, prevents unnecessary biopsies, and uses fewer cores, but there is still concern for infection.2 Because transrectal biopsies pass the needle through the rectum, each pass poses a risk of introducing rectal flora into the prostate and/or urethra. To mitigate the risk of infection, an enema and prophylactics, typically fluoroquinolones, are administered prior to biopsy. Although effective, the widespread use of fluoroquinolones is threatening our ability to treat bacterial infections.1
Rising Infection Rates
“From 1996 to 2005 the rate of readmission for sepsis post-transrectal biopsy in Canadian men rose from 0.6% to 3.6%.”4
Fluoroquinolone resistant bacteria, which is responsible for most cases of sepsis, is often greater in patients post-transrectal prophylactics than prior.3 In 2016, the FDA announced that fluoroquinolones should only be used as a last resort due to the risk of “disabling and potentially permanent side effects of the tendons, muscles, joints, nerves, and central nervous system that can occur together in the same patient”.1 As a result, transrectal biopsy prophylactics now encompass other broad spectrum antibiotics such as multi-drug prophylactics or culture-specific prophylactics. These methods may be successful, resulting in a less than 1% sepsis rate, but they directly contradict the warnings from the CDC and WHO by using more or more powerful antibiotics.1
The Transperineal Approach- Why The Uptake Is Slow
“The rate of sepsis post-transperineal biopsy is nearly 0%, which is 40 to 70 times less than that of transrectal.”4
Addressing Perceived Issues: Learning Curve, Procedure Time and Detection Rates
“It (transperineal biopsy) is becoming widely accepted as the superior method for targeting the anterior and apical regions, even in an MRI-targeted context.”1
The MRI-US fusion transperineal biopsy has the potential to become the new “gold standard” as it addresses both major concerns of accuracy and infection.2 It is becoming widely accepted as the superior method for targeting the anterior and apical regions, even in an MRI-targeted context.1,5,9 Sampling through the perineum also results in longer core lengths, which provides more prognostic information from the biopsy. Some studies have even shown MRI-US fusion transperineal biopsies to outperform the transrectal approach, by as much as 10%.9 Compared to transrectal biopsies, where the probe may be moved in the pitch, yaw and rotational directions, transperineal ultrasound probes are limited to rotation, which may reduce patient discomfort and overall movement.8
General vs. Local Anesthesia
“20% of patients refused to undergo biopsy without anesthesia, thus making effective anesthesia an important factor for successful biopsies.”11
To Sum It All Up
The Fusion Bx: A Simple All-in-One Prostate Biopsy Solution
Whether taking the transrectal or transperineal approach, Focal Healthcare’s Fusion Bx is the simple MRI-targeted fusion prostate biopsy solution. The unique semi-robotic arm allows freehand-like access to the entire gland, while maintaining consistent probe pressure on the prostate to minimize prostate deformation. The hands-free counterbalance keeps the probe steady in any position, which reduces the need for additional assistance. Using buttons on the stepper, physicians can advance through the simplified 4-step guided workflow without having to take their hands off the probe. Patient movement is typically more prevalent in biopsies, whether transrectal or transperineal, when performed under local anesthesia. Using our motion compensation feature, any movement is automatically adjusted for by maintaining MRI-US coupling, so procedures may continue uninterrupted.
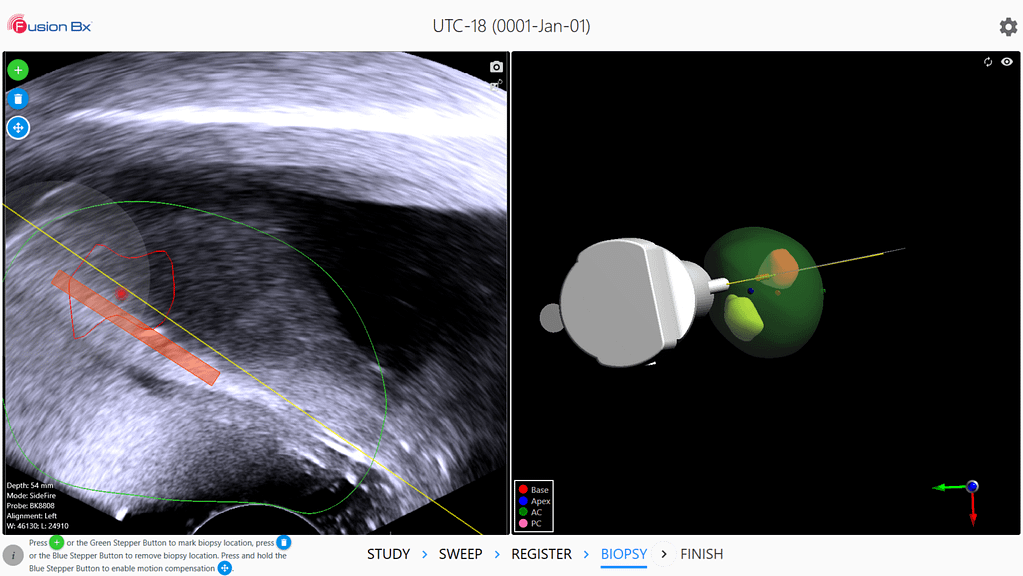
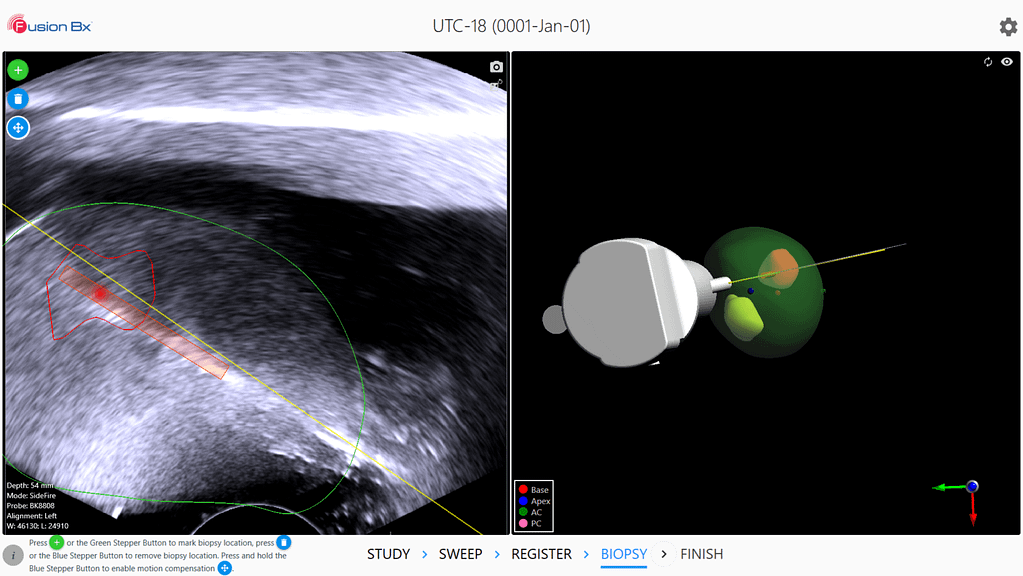
As the likelihood for needle deflection increases with the distance and mass the needle must pass through, the ability to account for deviation is even more important with transperineal biopsies. Compared to other systems, the Fusion Bx software displays the live ultrasound view, in addition to the 3D model, which shows the projected needle path and core locations. By visualizing the difference between the projected and actual needle path, physicians can more accurately account for any needle deflection (Fig.4- 5).
1 Grummet, J., Pepdjonovic, L., Huang, S., Anderson, E., & Hadaschik, B. (2017). Transperineal vs. transrectal biopsy in MRI targeting. Translational Andrology and Urology, 6(3), 368–375. doi: 10.21037/tau.2017.03.58
2 Xiang, J., Yan, H., Li, J., Wang, X., Chen, H., & Zheng, X. (2019). Transperineal versus transrectal prostate biopsy in the diagnosis of prostate cancer: a systematic review and meta-analysis. World Journal of Surgical Oncology, 17(1). doi: 10.1186/s12957-019-1573-0
3 Zowawi, H. M., Harris, P. N. A., Roberts, M. J., Tambyah, P. A., Schembri, M. A., Pezzani, M. D., … Paterson, D. L. (2015). The emerging threat of multidrug-resistant Gram-negative bacteria in urology. Nature Reviews Urology, 12(10), 570–584. doi: 10.1038/nrurol.2015.199
4 Grummet, J. P., Weerakoon, M., Huang, S., Lawrentschuk, N., Frydenberg, M., Moon, D. A., … Murphy, D. (2014). Sepsis and ‘superbugs’: should we favour the transperineal over the transrectal approach for prostate biopsy?. BJU International, 114(3). doi: 10.1111/bju.12536
5 Patel, P. (2020, February). The case for transperineal prostate biopsy vs. the transrectal approach. Urology Times, 48(2), 16–17.
6 Gross, M. D., Alshak, M. N., Shoag, J. E., Laviana, A. A., Gorin, M. A., Sedrakyan, A., & Hu, J. C. (2019). Healthcare Costs of Post-Prostate Biopsy Sepsis. Urology, 133, 11–15. doi: 10.1016/j.urology.2019.06.011
7 Ito*, M., Kataoka, M., Takemura, K., Suzuki, H., Sakamoto, K., Nakanishi, Y., … Koga, F. (2019). Mp13-11 Learning Curves, Cancer Detection Rates, And Complications Of Transperineal Prostate Biopsy Under Local Anesthesia By Trainee Urologists. Journal of Urology, 201(Supplement 4). doi: 10.1097/01.ju.0000555224.35839.bf
8 Tzeng, M., Cricco-Lizza, E., Awamlh, B. A. H. A., Pantuck, M., Margolis, D. J., Yu, M., & Hu, J. (2019). IDEAL Stage 2a experience with in-office, transperineal MRI/ultrasound software fusion targeted prostate biopsy. BMJ Surgery, Interventions, & Health Technologies, 1(1). doi: 10.1136/bmjsit-2019-000025
9 Wallis, C. (2019, May). AUA 2019: Transperineal vs. Transrectal MRI/US Fusion for Prostate Cancer Detection.
10 Bass, E. J., Donaldson, I. A., Freeman, A., Jameson, C., Punwani, S., Moore, C., … Ahmed, H. U. (2017).Magnetic resonance imaging targeted transperineal prostate biopsy: a local anaesthetic approach. Prostate Cancer and Prostatic Diseases, 20(3), 311–317. doi: 10.1038/pcan.2017.13
11 Ding, X.-F., Huang, T.-B., Lu, S.-M., Tao, H.-Z., Ye, X.-F., Wang, F., … Luan, Y. (2019). Pelvic plexus block to provide better anesthesia in transperineal template-guided prostate biopsy: a randomised controlled trial. BMC Urology, 19(1), 63. doi: 10.1186/s12894-019-0496-y
12 Kasivisvanathan, V., Rannikko, A. S., Borghi, M., Panebianco, V., Mynderse, L. A., Vaarala, M. H., . . . Moore, C. M. (2018). MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. New England Journal of Medicine, 378(19), 1767–1777. doi:10.1056/nejmoa1801993
13 Tu, X., Liu, Z., Chang, T., Qiu, S., Xu, H., Bao, Y., … Wei, Q. (2019). Transperineal Magnetic Resonance Imaging–Targeted Biopsy May Perform Better Than Transrectal Route in the Detection of Clinically Significant Prostate Cancer: Systematic Review and Meta-analysis. Clinical Genitourinary Cancer, 17(5). doi: 10.1016/j.clgc.2019.05.006